Bachelor of Science in Tourism Management
STI College Global City

As the eldest child in my family, I’ve cultivated a strong sense of responsibility and leadership from a young age. My curiosity and love for learning, whether through exploring digital tools or engaging with creative content, have shaped me into a resourceful and adaptable individual.
Professionally, I specialize in accurate and efficient insurance verification and prior authorization support. With over five years of customer service experience, including four years supporting U.S.-based healthcare accounts, I am committed to ensuring precise patient information and facilitating seamless medical processes. I take pride in being detail-oriented, organized, and dedicated to creating positive experiences for both patients and providers.
I am highly self-motivated, able to work independently, and thrive in fast-paced environments that require multitasking and problem-solving. I approach each task with diligence and a focus on delivering results while embracing new challenges.
I am excited to bring my skills, experience, and dedication to contributing to your team’s success.


STI College Global City
I conduct outbound calls to providers for medical authorizations and patient eligibility verification. I monitor prior authorization statuses, document communications per standards, ensure HIPAA compliance, and update authorization statuses and the Admin File Tracker to maintain accurate records and protect patient confidentiality.
I am responsible for communicating with medical providers, health insurance companies, attorneys, and lien holders via phone, fax, and email; negotiating lien resolution within firm-set parameters for clients; updating clients on case status; and organizing, collecting, and documenting sensitive personal information.
Entering patient information into a customer information system, ensuring customer satisfaction by addressing health-related issues and concerns, staying informed about plan changes, providing members and healthcare practitioners with information about benefits, and canceling members' plans as per their requests.
Receiving incoming calls from customers, identifying their needs or issues, and seizing opportunities to upsell products. It also involves reviewing and verifying transactions to ensure they meet quality standards, following up on unresolved customer inquiries, and building lasting customer relationships by going the extra mile in service.
Managing incoming calls and addressing customer service inquiries. This includes opening customer accounts, processing order overrides for eligible members, replacing orders in cases of damage or loss, notifying members about eligibility and benefits, and identifying and resolving customer needs and issues. Additionally, tracking orders and packages is an essential part of this job.
SEO-optimized content, conducts in-depth research, and ensures content ranks high on search engines.
Manages customer inquiries, generates sales leads, processes orders, and ensures high customer satisfaction.
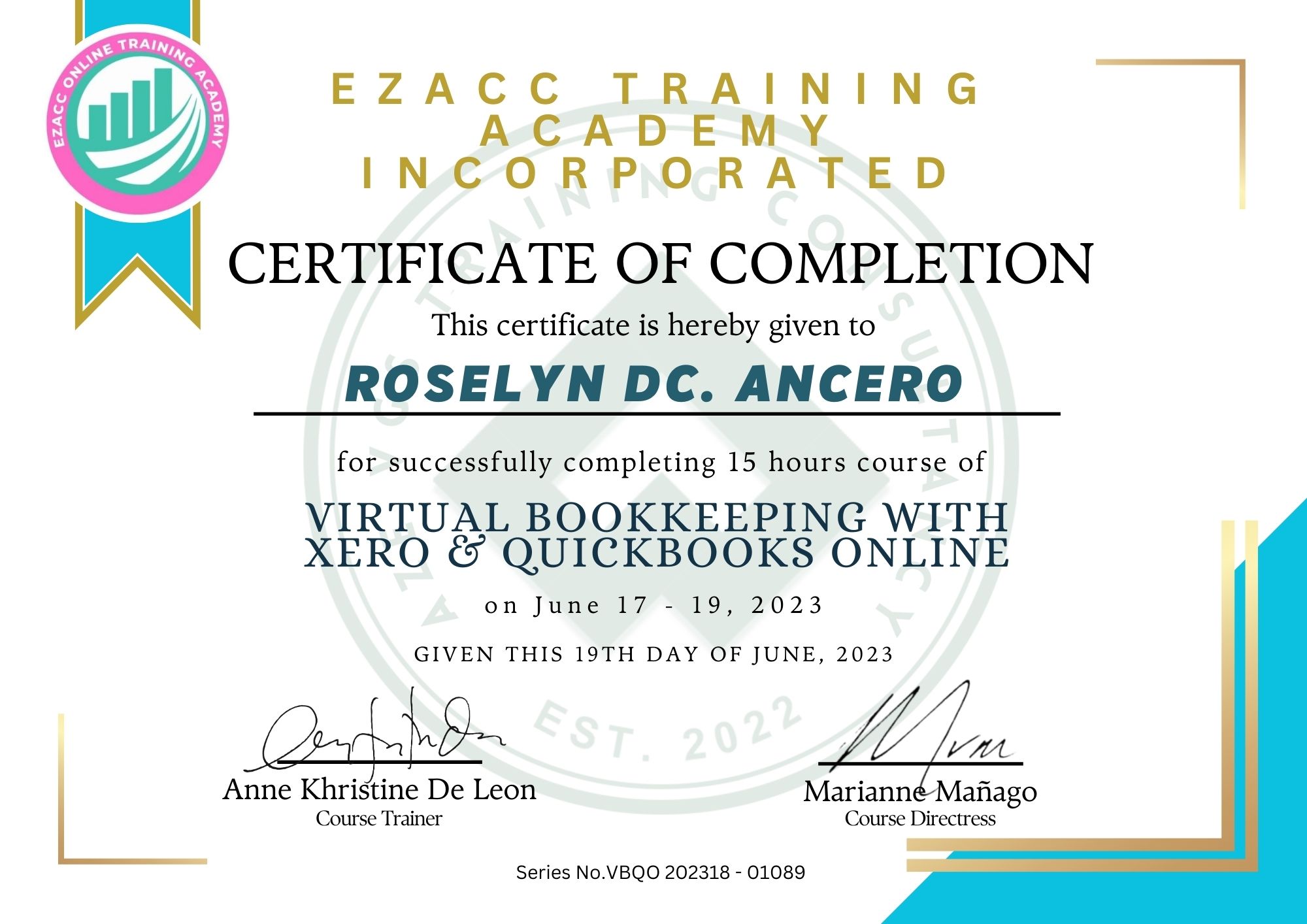
Efficient bookkeeping services for accurate financial records and informed business decisions.
Search the Internet for information on a wide variety of topics.
Make outbound calls for medical authorization, eligibility, track statuses, ensure HIPAA compliance, and update records.